Osteoporosis Explained: Protecting Your Bones as You Age
Osteoporosis is a silent but serious health condition that weakens bones and makes them more likely to fracture. Often developing without any noticeable symptoms, osteoporosis typically reveals itself only after a fall or a sudden fracture. While commonly associated with older women, this condition can affect anyone, including men and younger adults.
With nearly 10 million Americans already diagnosed and another 44 million at risk, understanding osteoporosis is critical for protecting your health and independence as you age.
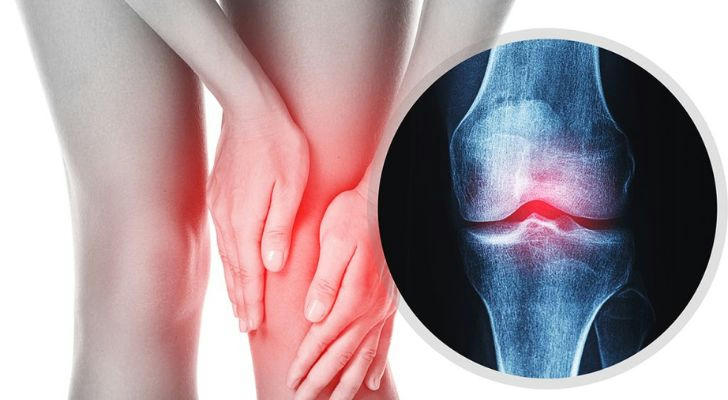
What Is Osteoporosis?
The word "osteoporosis" literally means "porous bones." Healthy bones have a honeycomb-like structure, but when affected by osteoporosis, the spaces in the bone become larger, reducing bone density and strength. As a result, even a minor fall or bump can lead to a fracture.
The condition most often affects the hips, spine, and wrists. Spinal fractures are particularly dangerous because they can occur without any noticeable trauma, sometimes just from bending or lifting.
Key Risk Factors
Osteoporosis can develop from a combination of factors, many of which are preventable. Understanding your risk profile is the first step toward prevention.
- Age: Risk increases significantly after age 50.
- Gender: Women are more susceptible due to lower bone mass and menopause-related hormone changes.
- Genetics: Family history of osteoporosis or fractures increases your risk.
- Lifestyle: Sedentary behavior, smoking, and excessive alcohol use can all contribute.
- Medical conditions: Rheumatoid arthritis, thyroid disorders, and certain cancers can affect bone density.
- Medications: Long-term use of corticosteroids or anticonvulsants may weaken bones.
Signs and Symptoms to Watch For
Osteoporosis is often symptomless until a fracture occurs. However, some signs that may indicate weakening bones include:
- Loss of height over time
- A stooped posture
- Chronic lower back pain
- Fragility fractures (especially in the spine, hips, or wrists)
- Bones breaking more easily than expected
Because it can go undetected for years, routine screening is essential—especially if you’re over 65 or have other risk factors.
Diagnosis: How Doctors Detect Osteoporosis
The gold standard for diagnosing osteoporosis is a DEXA (dual-energy X-ray absorptiometry) scan. This test measures bone mineral density (BMD) and compares it to the average for a healthy young adult.
You may also undergo:
- Blood tests to rule out other causes of bone loss
- FRAX score evaluation to assess fracture risk
How to Prevent and Manage Osteoporosis
Fortunately, osteoporosis is both preventable and manageable. Early intervention is key to avoiding long-term damage.
1. Focus on Bone-Strengthening Nutrition
- Calcium: Adults over 50 should get 1,200 mg/day. Best sources include dairy (milk, yogurt, cheese), leafy greens (collard greens, kale), and fortified products (orange juice, tofu).
- Vitamin D: Required for calcium absorption. Aim for 600–800 IU/day from sunlight, fatty fish (salmon, mackerel), or supplements.
- Protein: Supports bone repair. Include lean meat, legumes, and eggs in your meals.
- Magnesium, phosphorus, and zinc: Found in nuts, seeds, and whole grains—these also play roles in bone metabolism.
2. Exercise Regularly to Build Bone
Weight-bearing and resistance exercises are vital:
- Weight-bearing: Walking, hiking, dancing, stair climbing
- Resistance training: Light weight lifting, resistance bands
- Balance exercises: Tai Chi or yoga to reduce fall risk
Aim for 150 minutes of moderate activity per week, plus two strength sessions.
3. Lifestyle Changes That Make a Difference
- Quit smoking: Smoking reduces bone mass and disrupts hormone function.
- Limit alcohol: No more than one drink/day for women or two for men.
- Prevent falls: Install handrails, wear supportive footwear, remove loose rugs, and keep rooms well-lit.

4. Medications for Bone Health
Doctors may prescribe medications to strengthen bones or slow bone loss:
- Bisphosphonates: First-line treatment (e.g., alendronate, risedronate)
- Denosumab: A biannual injection to reduce bone breakdown
- Selective estrogen receptor modulators (SERMs): Mimic estrogen’s bone-protecting effects
- Hormone therapy: Occasionally used for postmenopausal women
- Anabolic agents: Like teriparatide, which helps grow new bone
Always discuss potential side effects and whether these medications are right for you.
How Health Insurance Supports Osteoporosis Care
Bone health can be expensive without proper coverage. Fortunately, most insurance plans include:
- Annual DEXA scans (especially for people over 65 or at high risk)
- Specialist visits (endocrinologists or rheumatologists)
- Prescription drugs (depending on plan tier)
- Rehabilitation and fall prevention programs
- Supplement coverage: Some plans cover calcium or vitamin D supplements if prescribed
If you're unsure whether your policy covers bone density tests, check directly with your insurer or Medicare plan provider.
When to Talk to Your Doctor
Speak with your doctor if you:
- Have a history of fractures
- Are a woman over 50 or a man over 70
- Experience loss of height, posture changes, or chronic back pain
- Take medications that impact bone health
- Have conditions like diabetes or hyperthyroidism
Conclusion: Protect Your Bones for a Healthier Future
Osteoporosis doesn’t have to lead to a fractured future. Through a combination of proper diet, regular exercise, lifestyle changes, and early medical intervention, you can keep your bones strong and resilient.
As you age, maintaining your skeletal health is just as important as your heart or lungs. Don’t wait for a fracture to take action. Prioritize your bone health today—because strong bones mean a strong foundation for the rest of your life.